Can A Trans Woman Still Produce Sperm? Exploring Fertility

A trans woman who has undergone gender-affirming surgery typically cannot produce sperm. Those who have not had surgery may still retain their sperm-producing capability.
Transgender issues are increasingly recognized in today’s society, leading to greater understanding and acceptance. Trans women are individuals assigned male at birth who identify and live as women. Their reproductive abilities can vary significantly based on personal medical choices. Some may undergo hormone therapy or surgeries that impact fertility.
Understanding these nuances is crucial for discussions about family planning and reproductive health. This topic is not just a medical issue but also deeply intertwined with identity, rights, and personal choices. Awareness and education can foster empathy and support for trans individuals navigating these complex realities.
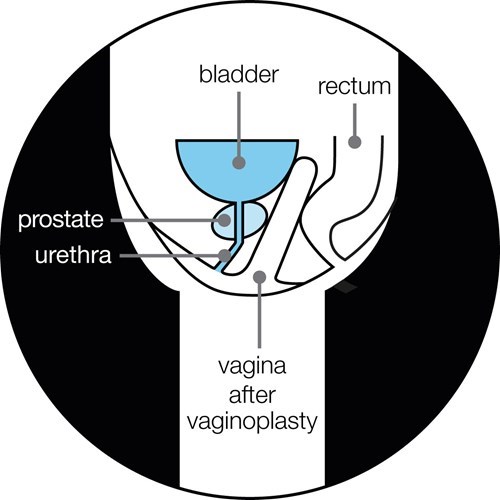
Credit: prostatecanceruk.org
Biological Basis Of Fertility In Trans Women
The biological basis of fertility in trans women is complex. It involves understanding how hormone therapy and physical changes affect reproductive functions. Many trans women wonder if they can still produce sperm after transitioning. This section explores the key factors influencing fertility in trans women.
Hormonal Influence On Reproductive Functions
Hormones play a crucial role in fertility. Trans women typically undergo hormone therapy, which includes:
- Estrogen: Promotes female secondary sexual characteristics.
- Anti-androgens: Reduce testosterone levels in the body.
These hormonal changes can impact sperm production. Studies show:
| Hormone | Effect on Sperm Production |
|---|---|
| Estrogen | Can decrease sperm production. |
| Anti-androgens | Can significantly lower testosterone, affecting sperm. |
Some trans women may retain the ability to produce sperm. Regular monitoring of hormone levels is essential. Consulting with a healthcare provider helps understand individual circumstances.
Physical Changes During Transition
Transitioning involves physical changes that impact fertility. Key changes include:
- Development of breast tissue.
- Redistribution of body fat.
- Reduction in testicular size.
These changes can affect the reproductive system. Sperm production may decline as hormone therapy progresses. Some trans women choose to bank sperm before starting hormone treatment. This option preserves fertility for future use.
Understanding these factors helps trans women make informed choices. Knowledge about fertility options is vital for family planning.
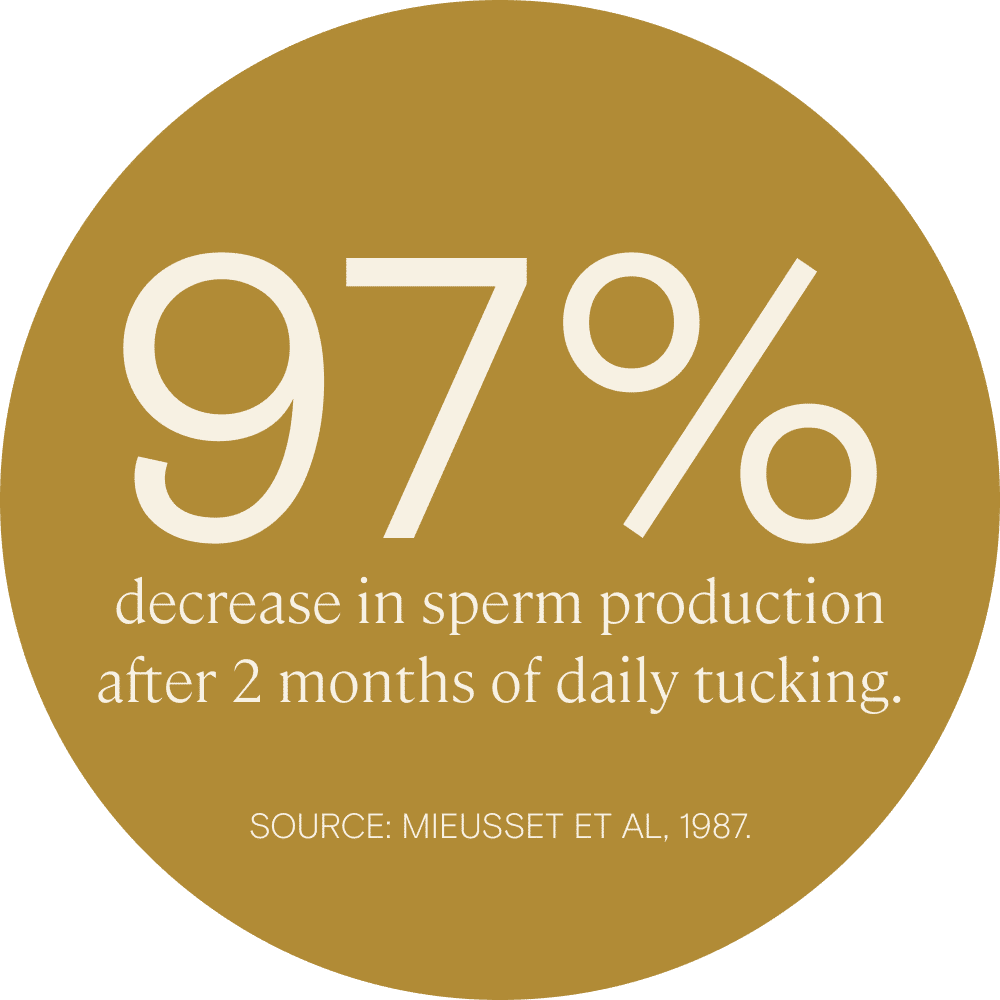
Credit: www.givelegacy.com
Impacts Of Hormone Replacement Therapy
Hormone Replacement Therapy (HRT) plays a significant role in a trans woman’s transition. HRT usually includes estrogen and sometimes anti-androgens. These hormones can affect many aspects of the body, including sperm production. Understanding these impacts is essential for those considering HRT.
Effects Of Estrogen On Sperm Production
Estrogen has several effects on the body. It can significantly influence sperm production. Here are key points to consider:
- Estrogen reduces testosterone levels.
- Lower testosterone affects sperm count.
- Prolonged exposure can lead to infertility.
Studies show that many trans women experience a decrease in sperm production after starting HRT. The body begins to prioritize female characteristics, which can halt sperm generation.
Possibility Of Reversibility After Hrt
Some individuals wonder about the reversibility of HRT effects. Research suggests that:
- Stopping HRT may allow some recovery of sperm production.
- Recovery depends on the duration of HRT.
- Younger individuals may have better chances of recovery.
Consulting a healthcare provider is crucial. They can provide personalized advice and options for fertility preservation before starting HRT.
Sperm Preservation Options
Sperm preservation offers important choices for trans women. These options help maintain fertility before transitioning. Understanding these methods is vital for future family planning.
Cryopreservation Before Transition
Cryopreservation is a common method for preserving sperm. Here are some key points:
- Timing: It’s best to preserve sperm before starting hormone therapy.
- Process: Sperm is collected, analyzed, and frozen.
- Storage: Frozen sperm can last for many years.
This method allows trans women to have biological children later. It ensures options remain open after transitioning.
Fertility Preservation Counseling
Fertility preservation counseling provides support and information. Important aspects include:
- Assessment: Evaluating individual health and fertility potential.
- Options: Discussing various sperm preservation methods.
- Emotional Support: Addressing feelings about fertility and transition.
Counseling helps individuals make informed decisions. It offers clarity on available options and next steps.
| Method | Description | Benefits |
|---|---|---|
| Cryopreservation | Freezing sperm for future use | Long-term storage, preserves fertility |
| Storage Facilities | Specialized clinics maintain frozen sperm | Safe and secure environment |
Future Of Fertility In Transgender Medicine
The future of fertility in transgender medicine is evolving rapidly. Innovations in science and technology are enhancing reproductive options for transgender individuals. Trans women, in particular, are exploring their fertility potential in new ways.
Understanding how medical advancements can help is crucial. Many trans women wonder about their ability to produce sperm. This section covers the latest innovations, legal, and ethical considerations in this field.
Innovations In Assisted Reproductive Technology
Assisted reproductive technology (ART) is transforming fertility options. New methods allow trans women to consider parenthood. Here are some key innovations:
- Sperm Banking: Trans women can freeze sperm before hormone therapy.
- IVF Techniques: In vitro fertilization helps in using stored sperm.
- Gene Editing: Techniques like CRISPR may improve genetic health.
- Artificial Insemination: This method offers alternative ways to conceive.
These technologies provide hope and possibilities for trans women. They can explore parenthood while maintaining their identity.
Legal And Ethical Considerations
Legal and ethical issues surround fertility for trans individuals. These factors impact their choices significantly. Here are some considerations:
| Consideration | Description |
|---|---|
| Parental Rights | Trans parents may face challenges in custody and rights. |
| Consent Laws | Informed consent is crucial before any procedure. |
| Discrimination | Trans individuals may encounter bias in healthcare. |
| Insurance Coverage | Not all plans cover ART for transgender individuals. |
Awareness of these issues is vital. Advocates push for change and inclusivity in reproductive health.
Transgender medicine continues to grow. Understanding fertility options empowers trans individuals. The journey to parenthood is becoming more accessible and inclusive.

Credit: www.nytimes.com
Frequently Asked Questions
Can A Trans Woman Produce Sperm After Transition?
Trans women typically do not produce sperm after undergoing hormone therapy and surgeries, which usually affect sperm production.
What Factors Affect Sperm Production In Trans Women?
Hormone therapy, surgical interventions, and individual health can significantly influence sperm production in trans women.
Is Sperm Banking An Option For Trans Women?
Yes, sperm banking is a viable option for trans women before starting hormone therapy or undergoing surgeries.
Can A Trans Woman Father A Child?
A trans woman can father a child if she has viable sperm stored prior to transitioning.
What Are The Alternatives For Trans Women Wanting Children?
Trans women can explore options like adoption, surrogacy, or co-parenting to have children.
Conclusion
Understanding the complexities of sperm production in transgender women is essential. While each case varies, the potential for sperm production is possible. Consulting with healthcare providers and specialists is crucial for personalized guidance. By fostering open discussions and staying informed, individuals can make informed decisions about their reproductive health.
